Dear reader,
July 1, 2021, marked the beginning of a new era for Medicaid in North Carolina. NC Medicaid officially transformed from a fee-for-service model to a managed care model. Under the new model, most Medicaid beneficiaries in our state now receive Medicaid services in a new way — through private health plans.
This is a big change. Big changes can cause confusion and anxiety, and they inevitably start off with wrinkles that need to be ironed out. Thankfully, Medicaid beneficiaries in our state were not left to navigate this change on their own.
Launched in April 2021, the NC Medicaid Ombudsman is an independent advocate for beneficiaries in Medicaid Managed Care. We solve problems for beneficiaries — at both an individual and systemic level — so they can get the quality health care they need.
This report summarizes our work and highlights some successes from our first nine months of operation. We are honored to do this important work on behalf of North Carolina’s Medicaid beneficiaries, and we look forward to continuing it in 2022 and beyond.
Angeleigh Dorsey
Director, NC Medicaid Ombudsman

Angeleigh Dorsey is the inaugural Director of the NC Medicaid Ombudsman and the Western Regional Manager of Legal Aid of North Carolina, which operates the Ombudsman in partnership with the Charlotte Center for Legal Advocacy and Pisgah Legal Services. Before assuming leadership of the Ombudsman in 2021, Dorsey directed Legal Aid’s statewide Senior Law Project since its launch in 2007. She joined Legal Aid as a Senior Managing Attorney in 2002. She is based in Asheville.
Listening to beneficiaries
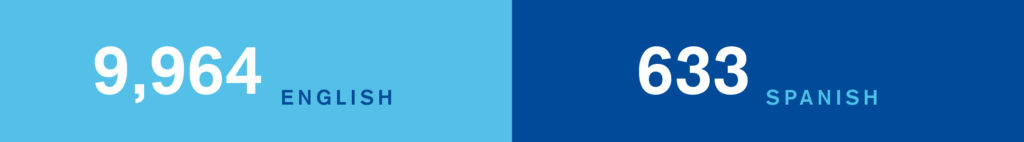
We answered 10,597 calls in Spanish and English.

Rosa’s* first language is Spanish. When she called her provider about a new hearing aid for her 13-year-old daughter, Rosa was told her request could not be accommodated because of the change to Medicaid Managed Care. A Spanish-speaking member of the NC Medicaid Ombudsman team called the clinic with Rosa, and helped resolve the issue. Rosa picked up her daughter’s hearing aid later that week.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Following through
We opened 6,714 cases, resolving 97% of them.


54-year-old Ali* is a refugee living with polio. He relies entirely on an electric wheelchair for mobility. When his wheelchair motor broke, he lost his independence. A local refugee agency tried to help Ali communicate with his primary care provider and health plan, but something was lost in translation. Documentation was never provided or escalated to repair Ali’s chair. The NC Medicaid Ombudsman helped Ali file a grievance with his health plan. A care manager swiftly stepped in, resulting in a new motor for Ali’s wheelchair just before Thanksgiving.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Educating and informing
We resolved 4,475 cases by educating and informing beneficiaries about Medicaid and managed care.


Jamal’s* three-year-old son has an uncommon genetic disorder that causes seizures several times a week. It took Jamal months to get an appointment with a pediatric neurologist who specializes in this condition. He had even made travel accommodations for the five-hour round trip. When the clinic called to cancel the appointment, he was crushed. When they said it was because the specialist was not included in his new health plan, he was furious. Jamal called the NC Medicaid Ombudsman for help. He told us that his family had moved several times recently, so they had not received any of the notices mailed to them about their transition to Managed Care. He had no idea that anything had changed about his family’s Medicaid coverage. In addition to providing Jamal with general information about Managed Care, our staff called the neurologist to explain that the program’s Transition of Care protections ensured that the appointment would be covered by Jamal’s health plan, even though the neurologist was an out-of-network provider. Thanks to our intervention, the neurologist reinstated the appointment for Jamal’s son.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Solving problems
We resolved 2,060 cases, solving specific problems for beneficiaries.


Tessa* had just left the NICU with her four-month-old baby when she learned his Medicaid coverage had been terminated. Because he was in “redetermination status,” the pediatrician who treated him from birth would be unable to provide care for him. Though well enough to leave the hospital, he had been born very premature and still had many health problems to address. Tessa called the NC Medicaid Ombudsman who discovered the baby’s status was due to a data error. The Ombudsman team escalated the matter for Tessa. NCDHHS was able to correct the error, enroll him in the right health plan and reconnect the baby with his pediatrician.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Partner with us!
- The NC Medicaid Ombudsman is always looking for community partners to help educate and empower NC Medicaid Managed Care beneficiaries.
- Ready to learn more? We will come to you. Use our online form to request an outreach event.
- Need material? We have a brochure, FAQ sheet and poster available for digital download in English and Spanish in the “For Community Partners” section of our website.
- Help us spread the word! Find our social media handles under “Contact Us“.