Dear Reader,
As we reflect on the past year, we are proud of the significant strides made in expanding Medicaid access and improving health care for North Carolinians. The successful implementation of Medicaid expansion, which has enrolled more than 650,000 new beneficiaries, represents a major milestone in the efforts to provide essential health care to those who need it most.
In July 2024, NC Medicaid launched the Behavioral Health and Intellectual/Developmental Disabilities Tailored Plan, a new NC Medicaid Managed Care plan that provides care to beneficiaries with serious mental health illness, severe substance use disorders, intellectual and developmental disabilities and traumatic brain injuries.
While there was much to celebrate in 2024, many of our neighbors suffered from the impacts from Hurricane Helene. Though it tore through North Carolina in one day, full recovery will take decades. Our hearts remain with those affected in Western North Carolina and we are committed to assisting survivors with connections to services.
The North Carolina Medicaid Ombudsman (NCMO) remains dedicated in our support for beneficiaries with guidance, assistance and advocacy as they navigate the NC Medicaid program. As we look toward the future, we are optimistic about the continued positive impact of these initiatives and our collective ability to build a healthier, more inclusive North Carolina.
Thanks for your support,
Katelyn Millette
Director, NC Medicaid Ombudsman

Katelyn Millette is director of the NC Medicaid Ombudsman. She took on the role in August 2023 after serving as the inaugural program manager for two years. Prior to the Ombudsman, she was with Legal Aid of North Carolina as assistant director of the HOPE Program, which provided rent and utility relief to North Carolinians during the pandemic. Millette is passionate about advocacy and serving NC Medicaid beneficiaries. She is proud to lead the hardworking and dedicated advocates of the NC Medicaid Ombudsman.
Listening to beneficiaries
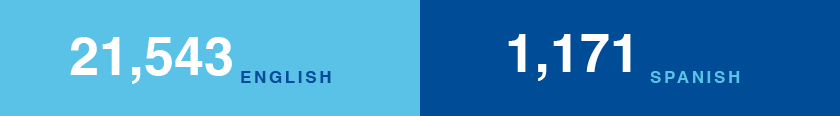
The NCMO handled 22,714 calls in English and Spanish.

Stephanie’s son, Max*, age 5, is an NC Medicaid beneficiary and needs allergy shots. The allergist’s team told Stephanie they could treat Max even though they did not accept his health plan.
After three weeks of injections, the allergist’s office sent Stephanie a bill for $2,000. When his health plan would not pay the doctor, they refused to see Max for his shots. Shocked and frustrated, Stephanie reached out to the NC Medicaid Ombudsman, who discovered there was miscommunication between the allergist’s front desk and billing department.
The Ombudsman explained if a doctor’s office gives incorrect information to a Medicaid beneficiary about coverage or payment, the patient is not responsible for the bill. The doctor waived all but $45 of the balance and resumed giving Max his allergy shots.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Following through
The NCMO opened 19,073 cases and 95% of them were resolved.


When he received a diagnosis of thyroid cancer, Kelvin* was put on a waiting list for radiation treatment. Shortly after he was scheduled to receive his first dose, his appointment was canceled because his NC Medicaid renewal was not processed in time.
Kelvin’s doctor told him if the issue wasn’t resolved soon, he would be placed back on the waitlist, which would be months.
Kelvin’s twin brother, Keith, called the NC Medicaid Ombudsman, who escalated the case to NC Medicaid. Kelvin was put back on the waitlist and will get the care he needs. Keith thanked us and said, “Without your help, I may have lost my brother and best friend.”
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Providing support and referrals
When beneficiaries need additional help, the NCMO connects them to our partners for information and resources.


Marjorie is the proud mother of two girls, Aubrey, age 8 and Angel*, age 18 months. Angel has Krabbe disease, a rare genetic condition that causes severe symptoms including seizures, hearing loss and nerve pain.
Angel’s doctors told Marjorie she would need a complex surgery in September. Marjorie was nervous how the launch of Tailored Plans would impact Angel’s Medicaid coverage and the upcoming procedure.
She contacted the NC Medicaid Ombudsman. The surgery was scheduled at Atrium Health/Wake Forest Baptist, but neither the hospital nor the pediatric surgeon was contracted with Angel’s Tailored Plan. The Ombudsman assisted with a formal legal referral for a current and possible long-term continuity of care issue. The Ombudsman worked to make sure all doctors were able to contract with Angel’s Tailored Plan. Angel got the surgery she needed and is back home with her sister and Marjorie.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Helping people access the right coverage
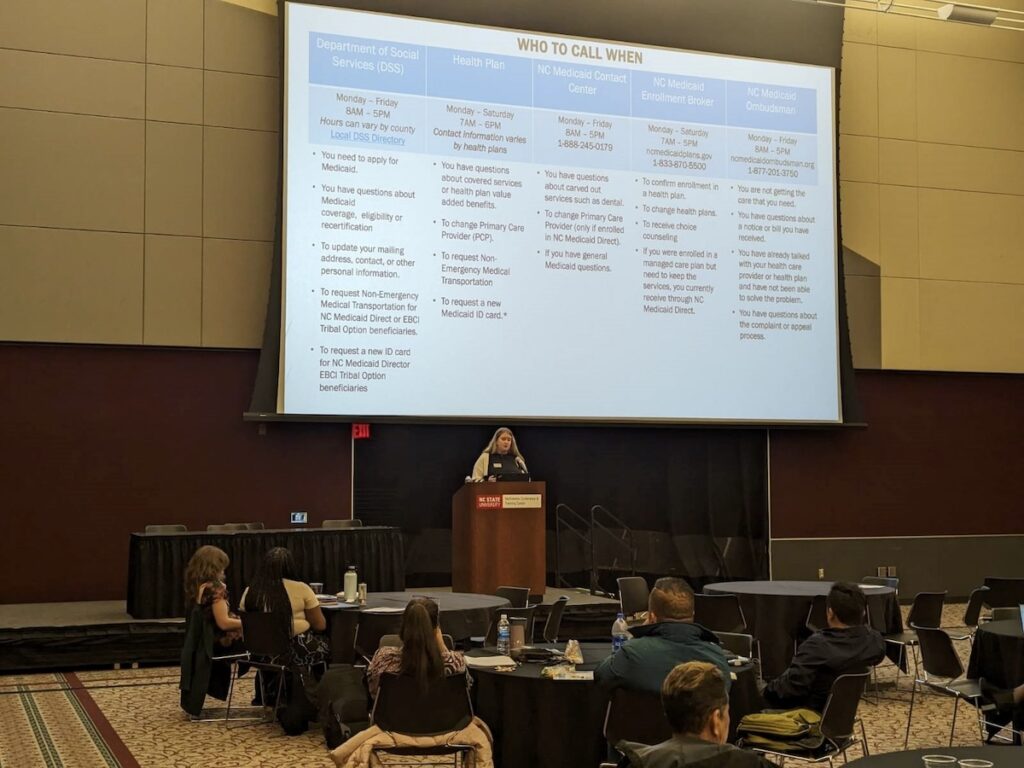
The NC Medicaid Ombudsman helps Medicaid beneficiaries with access to care. The team often gets calls about NC Medicaid eligibility. In these instances, we answer beneficiary questions and refer them to their local Department of Social Services Services for details about eligibility and to apply for coverage.


Becca* age 15, has a gastrointestinal condition that requires specialized care. When her foster care manager, Latoya, tried to make an appointment for her, she was told that Becca’s visit would be out-of-network.
Latoya knew Becca should be covered by NC Medicaid Direct but was told Becca was not eligible because she collects Social Security Income.
Latoya did not think this was correct, so she called the NC Medicaid Ombudsman, who escalated the issue to NC Medicaid and discovered Becca’s local Department of Social Services made a mistake. Becca was moved to NC Medicaid Direct and is feeling better.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Tracking historically systemic issues to assist with solutions
We highlighted challenges to NC Medicaid and facilitated solutions.


Camillo* works hard and does his best to manage his Type 1 diabetes. On his lunch break, he got a call from his pharmacy saying his insulin refill had been denied.
Camillo found the problem was third-party insurance and called his health plan several times for help. With no resolution and only one dose left, Camillo called the NC Medicaid Ombudsman.
The Ombudsman discovered that Camillo needed prior authorization for his insulin because his doctor was out-of-network.
In addition to removing the third-party insurance, the Ombudsman found a doctor that could submit the authorization so Camillo could fill his prescription. The Ombudsman told Camillo about Tailored Care Management and connected him to a care manager for support.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Outreach
The NCMO deepened connections with partners to increase outreach.

Virtual outreach

NC Medicaid Ombudsman webinars
The NC Medicaid Ombudsman offers a monthly webinar the third Wednesday of the month at 2 p.m. During the monthly webinar, attendees hear about the program and a highlighted topic. Register here.
“Meet the Plan” in partnership with Alliance Health
In collaboration with Alliance Health, the NC Medicaid Ombudsman offers a monthly “Meet the Plan” webinar. During the virtual sessions, attendees receive an overview of the programs and services both offer in English and Spanish. Learn more.
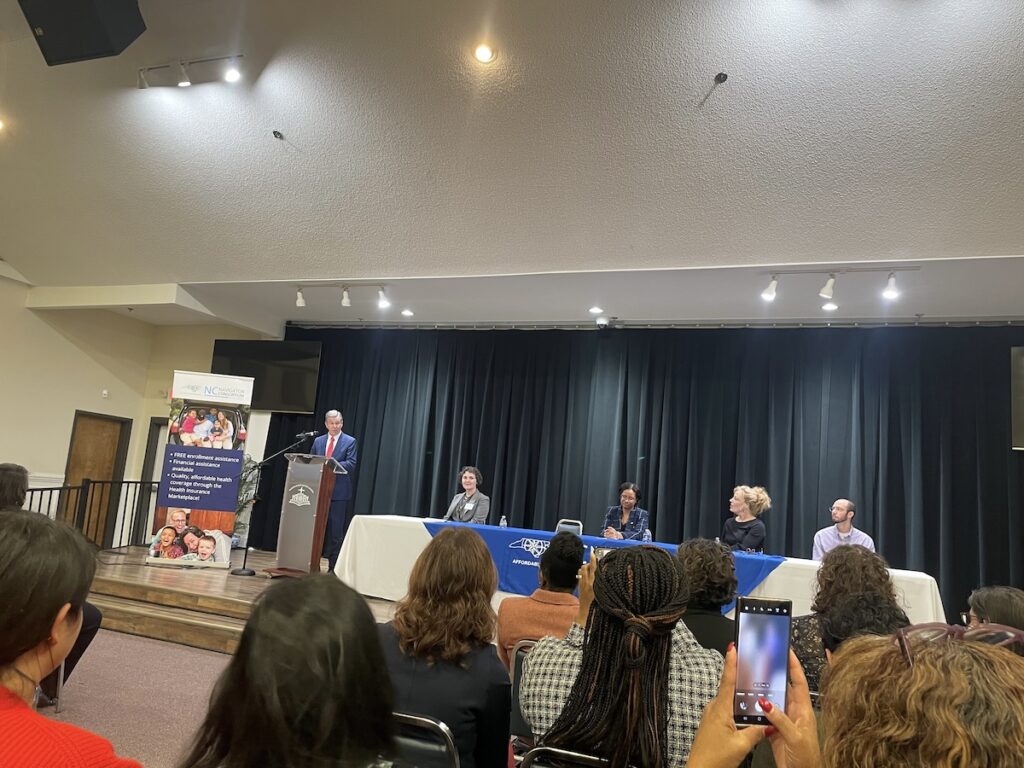
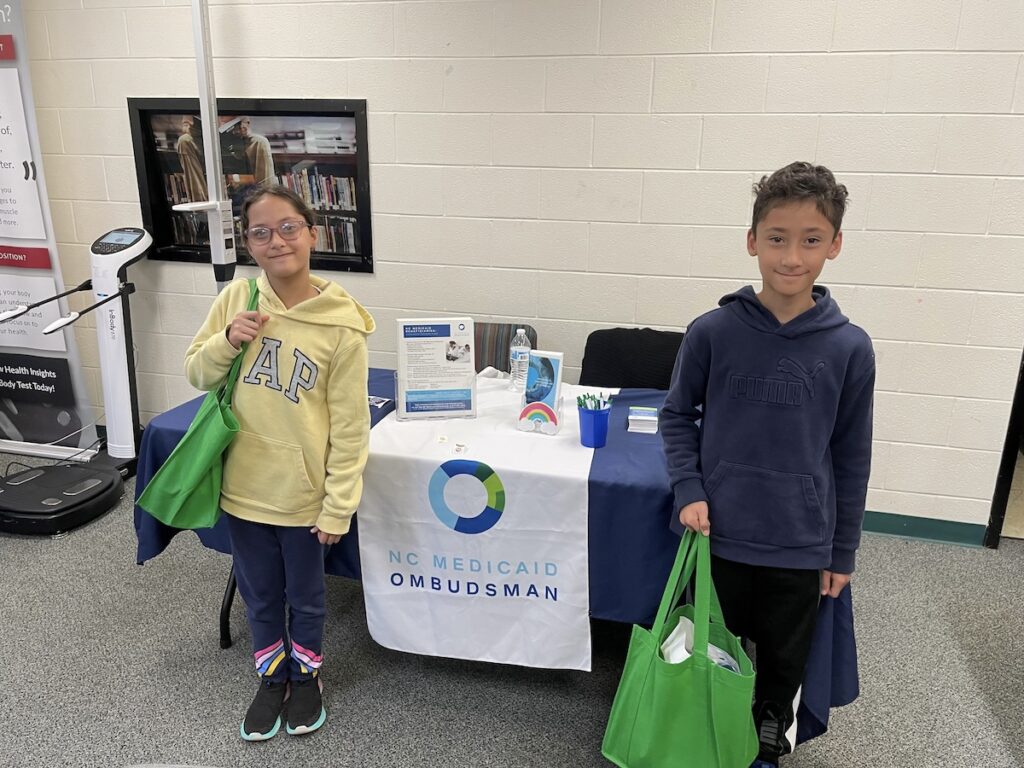
In-person outreach
Ready to learn more?
Request a virtual or in-person outreach event
The Ombudsman offers in-person and virtual educational sessions about the program and services that can be customized to the audience. To request a presentation or presence at a community event, send an email with your name, email address, phone number, organization name, county/counties of service, intended audience and whether in-person or virtual.
Request printed materials
To request printed materials, send an email with your name, email address, agency name, the address where the materials need to be sent, the quantity needed and languages desired.