Dear Reader,
As your advocate for quality health care, the NC Medicaid Ombudsman team was thrilled to see Medicaid expanded for adults ages 19 to 64 on Dec. 1, 2023. With expansion, NC Medicaid is expected to provide coverage to more than 600,000 additional North Carolinians. Raising the income eligibility threshold, Medicaid expansion has reduced the number of people who fall into the Medicaid gap – earning too much to qualify for Medicaid but too little to afford health insurance.
Using a “no wrong door” approach, it is the job of the NC Medicaid Ombudsman to support any Medicaid beneficiary in need of education, advocacy, referral or connection. We have been noticeably busier since the start of expansion, helping clients impacted by barriers to care, including improper data entry and problems with Medicaid ID cards. Ombudsman team members worked with other Medicaid business units to resolve challenges with health plan auto-enrollment and health care choice selection and issues surrounding non-emergency medical transportation (NEMT) for Medicaid-eligible individuals who need and request assistance with rides.
Across North Carolina, Medicaid expansion has created opportunities for our staff to deepen connections with current community partners and engage with new ones. This outreach has been deeply gratifying.
As we look forward to assisting additional expansion enrollees and the launch of Tailored Plans July 1, 2024, we are dedicated to continuing to fiercely advocate for NC Medicaid beneficiaries and their families.
Thanks for your support,
Katelyn Millette
Director, NC Medicaid Ombudsman

Katelyn Millette became director of the NC Medicaid Ombudsman in August 2023 after serving as the inaugural program manager for two years prior. Before joining the Ombudsman team, she worked for Legal Aid of North Carolina since 2019, most recently serving as assistant director of the HOPE Program, which provided rent and utility relief to North Carolinians during the pandemic. Millette is passionate about advocacy and serving NC Medicaid beneficiaries. She is proud to lead the hardworking and dedicated advocates of the NC Medicaid Ombudsman.
Listening to beneficiaries
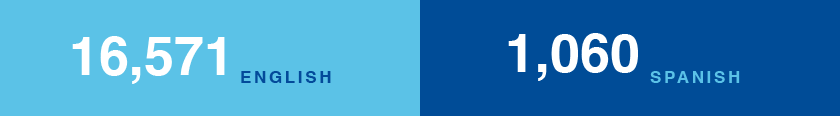
We answered 17,631 calls in English and Spanish.

Harold*, a NC Medicaid beneficiary, was near the end of his year-long battle with stage 4 colon cancer. With the support of his oncology team, he chose to end treatment and opt for hospice and palliative care. The only hospice provider in Harold’s area accepted Healthy Blue, but not his current NC Medicaid Managed Care health plan. When Harold was told he could not change his health plan for a month, he called the NC Medicaid Ombudsman and explained he didn’t have that much time left. We worked with a supervisor to secure approval for the out-of-network service and Harold spent his remaining days at home surrounded by loving family and friends.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Following through
We opened 14,024 cases, with 99% resolved.


Heart disease runs in Latasha’s* family. Though she has worked hard to change her lifestyle, she was recently diagnosed with high blood pressure and a heart condition. Her NC Medicaid Managed Care health plan covered her medication, but when the dosage increased, it made her sick to her stomach.
Latasha realized it contained low levels of lactose she was unable to tolerate in a higher dose due to lactose intolerance. When she tried to alter the prescription through a compounding pharmacy, she was told it was cost prohibitive to produce. She turned to the NC Medicaid Ombudsman for help. One of our dedicated team members spent several weeks researching alternative prescriptions, and thankfully one worked! Now Latasha can comfortably get back to prioritizing her heart health.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Providing support and referrals
When beneficiaries needed more help, we connected them to our partners to get information and resources.


In addition to medical conditions that include allergies and asthma, nine-year-old Braiden* suffers from psychogenic non-epileptic seizures, events that look like seizures but are caused by acute emotional distress. His condition worsened after he and his mom, Brandy*, had to move into a hotel. After struggling to find therapists who could help Braiden, Brandy was finally referred to NCCARE360 for housing stability and they suggested she contact the NC Medicaid Ombudsman.
We learned Brandy was a NC Medicaid beneficiary and Braiden receives services from a Local Management Entity/Managed Care Organization (LME/MCO) that assists those with serious mental health and intellectual/developmental disability services.
Although Braiden was eligible for Tailored Plans, launching July 1, 2024, he had not been assigned a Tailored Care Manager to help coordinate care for his complex condition and find resources to help Brandy achieve stability. We advocated for the LME/MCO to assign a Tailored Care Manager who worked with them to find an apartment. Now that they have affordable housing that is clean and safe, Braiden is doing much better.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Identifying systemic issues
We highlighted challenges to NC Medicaid and facilitated solutions.

Consuelo* and her husband applied for NC Medicaid to get their children immunized and enrolled in school. However, when they received their ID cards from their health plan, they were wrong. The children’s first names were incorrect, their middle names were misspelled and their last names were shortened.
With Spanish as her primary language, Consuelo called the NC Medicaid Ombudsman for help. We were able to get the health plan to redesign and rebuild their card printing system to allow for a longer character limit and properly fit the children’s complete names on their ID cards. Consuelo received the new ID cards in time to get her children vaccinated and ready for the start of the school year.
*Names and some minor details have been changed to protect the confidentiality of those we serve.
Reaching out
Our teams deepened connections with partners to increase outreach.

Partner with us!
The NC Medicaid Ombudsman is always looking for community partners to help educate and empower NC Medicaid Managed Care beneficiaries.
Ready to learn more?
We will come to you. Use our online form to request an outreach event.
Need material?
We have materials available for digital download in English and Spanish in the “For Community Partners” section of our website.
Help us spread the word!
Find our social media handles under “Contact Us“.